镰刀菌属Fusarium Link.于1809年首次建立,目前归属于子囊菌门Ascomycota、盘菌亚门Pezizomycotina、粪壳菌纲Sordariomycetes、肉座菌目Hpyocreales、丛赤壳科Nectriaceae。自从1809年Link首先在锦葵科植物上发现第一株镰刀菌,定名粉红镰刀菌Fusarium roseum Link.以来,已识别出超过100种镰刀菌,但仅有一些种类可导致人类感染(Alastruey-Izquierdo et al. 2008)。茄病镰刀菌Fusarium solani是引起侵袭性疾病的最常见菌种(约占半数病例),其次是尖孢镰刀菌Fusarium oxysporum、轮枝镰刀菌Fusarium verticillioides(曾称为串珠镰刀菌Fusarium moniliforme),以及层生镰刀菌Fusarium proliferatum。其他报道较少的致病种包括单隔镰刀菌Fusarium dimerum、厚孢镰刀菌Fusarium chlamidosporum、甘蔗镰刀菌Fusarium sacchari、花腐镰刀菌Fusarium antophilum等。分子系统学研究表明,这些病原菌多为复合种,至少包含70种(O′Donnell et al. 2008;Balajee et al. 2009),这些复合种的临床意义仍不明确。它们分布极广,普遍存在于土壤及动植物有机体上,甚至存在于严寒的北极和干旱炎热的沙漠,属于兼寄生或腐生生活。
镰刀菌引起的人类感染种类繁多,包括皮肤及皮下组织感染、局部感染和播散性感染(又称侵袭性感染)。感染的临床形式取决于宿主的免疫状态和病原体进入的门户(Nucci & Anaissie et al. 2007)。本文对镰刀菌病的致病种、地域分布、危险因子、临床表现形式、药物敏感性及其诊断治疗进行了综述,旨在系统、全面了解该属真菌所致皮肤感染的特征。
1 镰刀菌感染的一般性描述
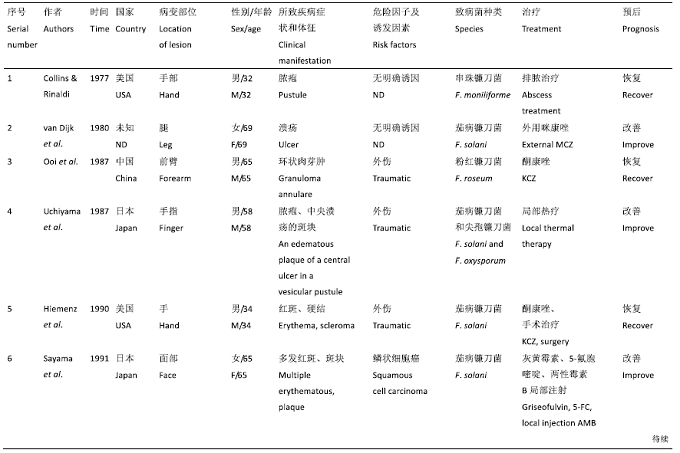
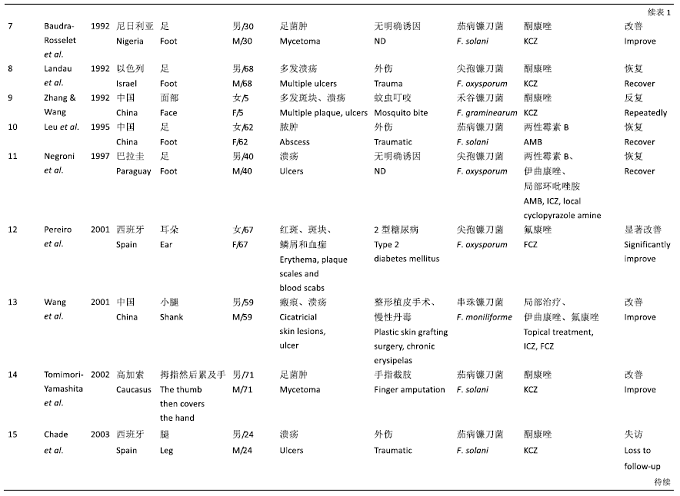
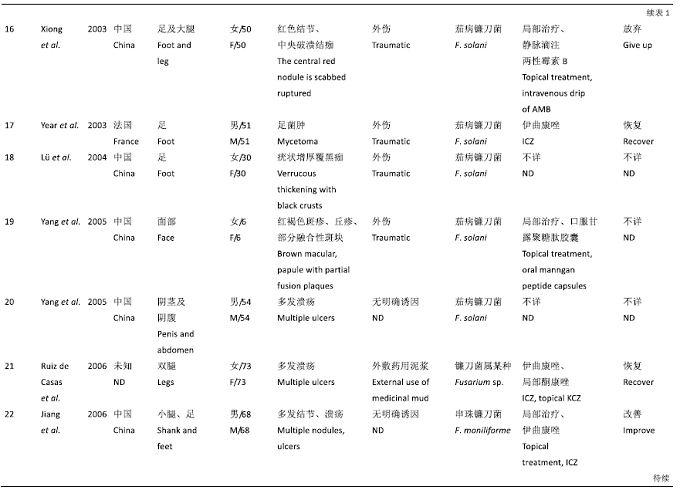
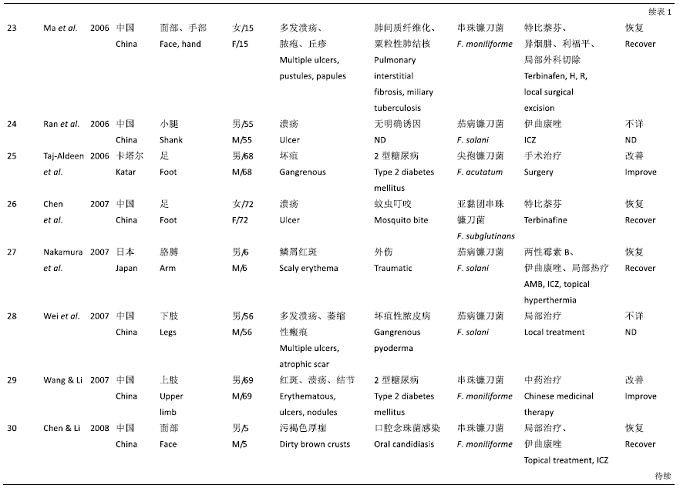
采用Excel建立数据库,检索自1970年至2018年发表的文献,记录其报道年份、年龄、性别、地区、致病菌菌种种类、临床表现、基础病/诱因、治疗、预后等。综合结果共获得47例英文病例报告,22篇中文病例报告,共计69例镰刀菌感染报告(表1,表2)。按照患者免疫功能状态进行划分,分为免疫正常患者和免疫低下(或)免疫缺陷的患者。免疫力低下(immunocompromised)主要由于免疫系统异常对机体不能发挥正常的保护作用,致使机体容易受到外界细菌、病毒等感染。长期严重的中性粒细胞减少(<0.5×109/L)和(或)严重免疫细胞缺陷,长期糖皮质激素、广谱抗生素、放疗、免疫抑制剂和细胞毒类药物的使用患者归为免疫低下(或)免疫缺陷的患者。
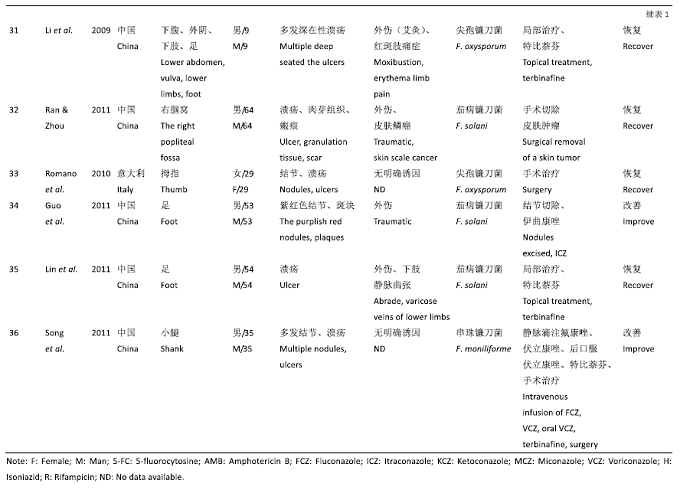
表1 免疫功能正常人群的皮肤镰刀菌感染的病例报道(1977-2018)
Table 1
|
|
|
|
|
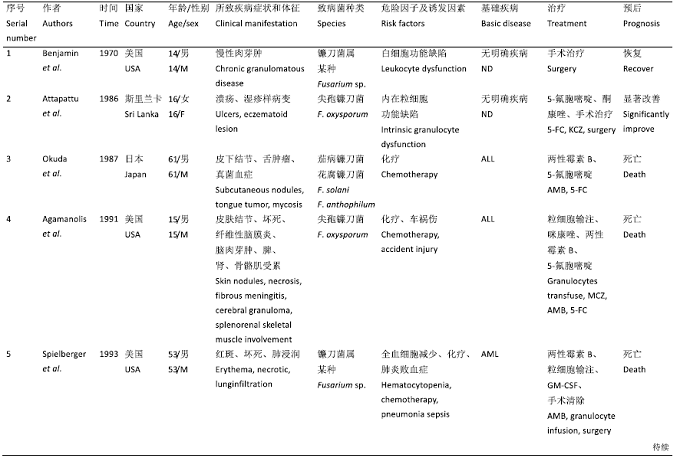
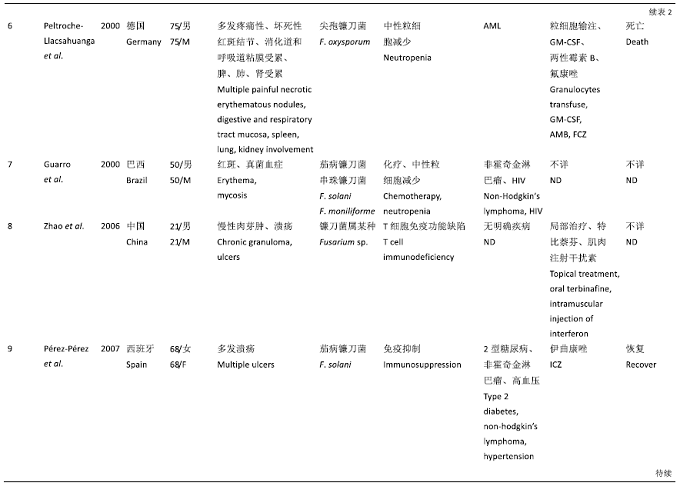
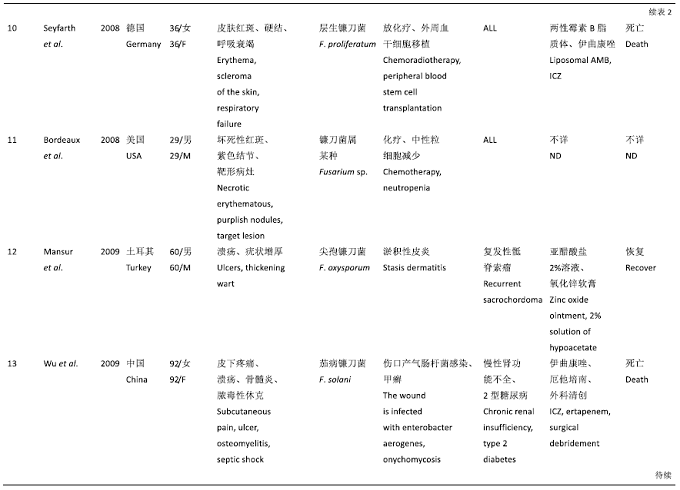
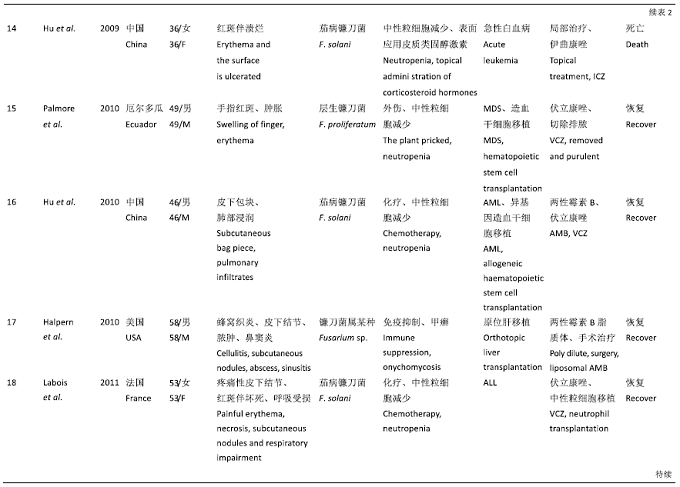
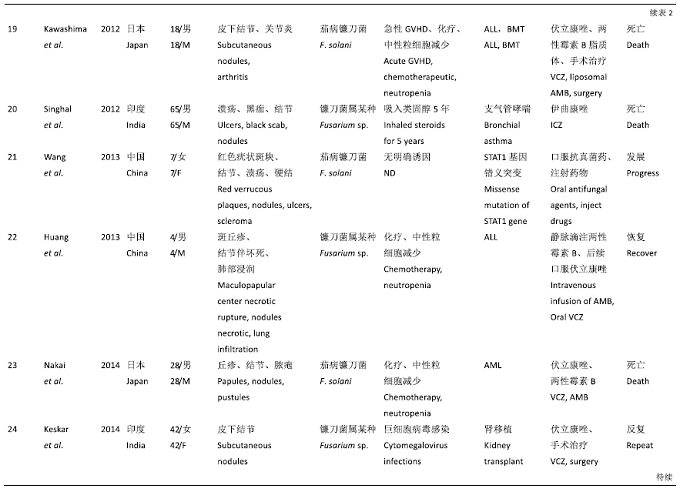
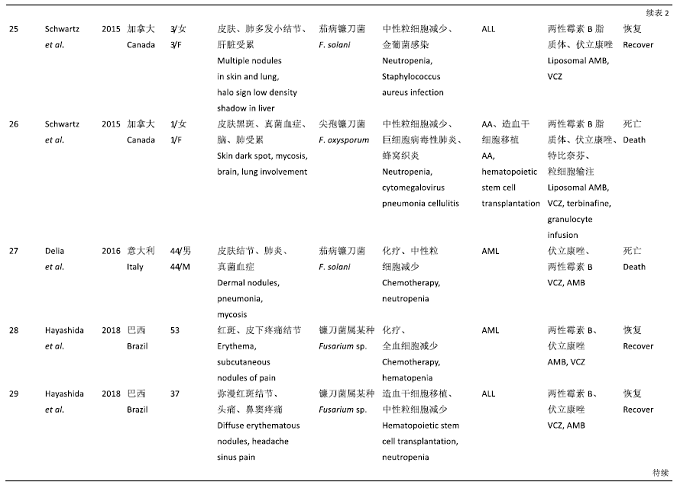
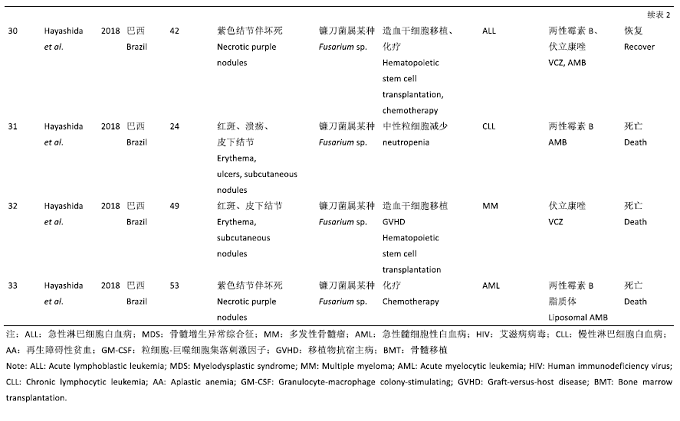
表2 免疫功能低下或缺陷的皮肤镰刀菌感染病例报道(1970-2018)
Table 2
|
|
|
|
|
|
|
2 年龄和性别分布
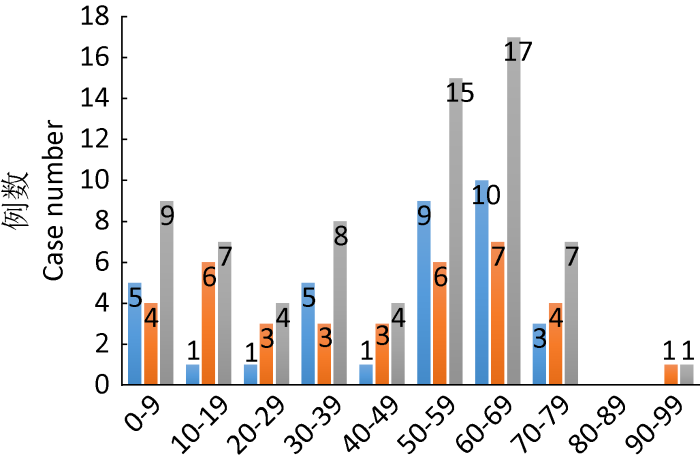
年龄范围总体跨度大,从1岁到92岁,平均年龄(43.09±22.54)岁(图1)。排除6例未查到性别的病例,其余男性41例,女性22例,男女比例为1.9:1。
图1
图1
镰刀菌致皮肤感染病例年龄分布柱状图
免疫正常患者; 免疫缺陷或低下患者; 所有患者
Fig. 1
Age distribution of Fusarium cases. Patients with normal immunity; Patients with immunodeficiency or immunosuppression; All patients.
3 地域分布
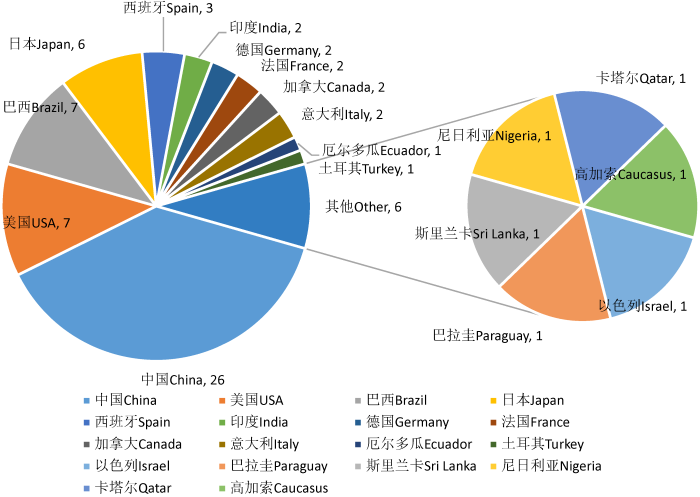
所研究的病例报道集中在亚洲国家,其中中国最多,有26例报道,美国报道了7例,巴西报道了7例,日本报道了6例,西班牙报道了3例,印度、德国、法国、意大利、加拿大各报道了2例,厄尔多瓜、土耳其、以色列、巴拉圭、斯里兰卡、尼日利亚、卡塔尔、高加索各报道了1例(图2),另有2例患者未查到地区。
图2
图2
镰刀菌致皮肤感染病例地域分布
中国报道镰刀菌致皮肤及皮下组织感染病例占比最高,达(26/69),其次是美国(7/69),再其次是巴西(7/69),然后是日本(6/69),其他国家分别为西班牙3例,印度、德国、法国、意大利、加拿大各2例,厄尔多瓜、土耳其、以色列、巴拉圭、斯里兰卡、尼日利亚、卡塔尔、高加索各1例
Fig. 2
Geographical distribution of Fusarium cases.
China reported cases of skin and subcutaneous tissue caused by Fusarium infection accounted for the highest, up to (26/69), followed by the United States (7/69), Brazil (7/69), Japan (6/69); three cases were reported in Spain; India, Germany, France, Italy and Canada reported two cases each; Ecuador, Turkey, Israel, Paraguay, Sri Lanka, Nigeria, Qatar and the Caucasus reported one case each.
4 临床表现形式
镰刀菌所致皮肤及皮下组织感染临床表现多种多样,在所收集的69例患者中,36例患者免疫功能正常,33例患者免疫功能低下或免疫缺陷(表3)。在免疫功能正常的宿主中,感染部位多局限于面部、手、足、四肢、耳朵及外阴皮肤,少数为泛发性感染。其中面部感染4例,分别表现为多发红斑斑块、多发溃疡、多发斑丘疹、污褐色厚痂。其中手部感染5例,手部感染多侵犯手指,其中4例表现为单发的脓疱、脓疱并伴溃疡的水肿性斑块、红斑硬结、结节伴溃疡,1例表现为足菌肿样改变。足部感染10例,其中3例单发溃疡,2例足菌肿,多发溃疡、脓肿、坏疽、结节斑块、疣状增厚各1例。上肢感染3例,其中2例分别表现为单发的肉芽肿病变、浸润性鳞屑红斑,1例表现为多发的坏死溃疡。下肢感染8例,其中5例表现为单发溃疡,3例表现为多发溃疡。耳部感染1例,表现为泛发的红斑斑块伴鳞屑、结痂。外阴局限性感染1例,表现为多发溃疡。其余患者表现为累及多部位的泛发性感染。在所有免疫功能正常的36例患者中,其中单发病变为21例,多发病变15例。皮疹类型以溃疡最多见,有21例(21/36)患者,约60%表现为单发或多发溃疡,多分布于下肢和足部。其余表现为红斑斑块7例、足菌肿2例、脓肿1例,脓疱、离心性肉芽肿、坏疽、疣状增厚覆黑痂、污褐色厚痂各1例。
表3 皮肤感染相关的镰刀菌病临床表现
Table 3
| 患病人群类型 Patient population type | 主要临床表现 Clinical manifestation | 病例数 Case load |
|---|---|---|
| 免疫力正常患者 Normal immunity people | 溃疡 Ulcer | 21 |
| 红斑 Erythema plaque | 7 | |
| 足菌肿 Mycetoma | 2 | |
| 免疫力低下或免疫缺陷患者 Immunodeficienty people | 仅皮肤受累 Only the skin is affected | 17 |
| 皮疹伴坏死 Rash with necrosis | 11 | |
| 皮疹不伴坏死 The rash is not accompanied by necrosis | 6 | |
| 皮肤合并系统性感染 Systemic infection | 16 | |
| 皮疹伴坏死 Rash with necrosis | 7 | |
| 皮疹不伴坏死 The rash is not accompanied by necrosis | 9 |
在免疫功能低下或免疫缺陷患者中,在严重和长期中性粒细胞减少的情况下最常见的表现是持续发热,对抗细菌和抗真菌治疗无效,其他表现包括鼻窦炎、肺炎、皮肤破损处的蜂窝织炎和转移性皮肤损伤、眼内炎、鼻眶脑真菌病、骨髓炎、真菌血症、肌炎、关节炎和中枢神经系统感染,以及累及脾、肾、肝脏等实体器官。在33例感染病例中,大部分患者有基础疾病,皮肤损伤可能是局限性的,也可能是泛发性的。局限性病变通常表现为创伤、甲真菌病或指间刺伤所致皮肤破裂部位的蜂窝织炎。泛发性病变患者可出现多发红斑丘疹或疼痛性结节病灶,常伴中央坏死,呈坏疽性脓皮病样外观。靶形病灶表现为在丘疹或结节病灶周围有1-3cm直径的薄红斑边缘,只有少部分患者存在,大疱非常少见。播散性镰刀菌病转移性皮损可累及任何部位,主要累及四肢,发展迅速,通常持续数天。大约三分之一(10/33)的免疫低下或免疫缺陷患者的皮损患者表现为不同发展阶段的病灶,包括丘疹、结节和坏死病灶。在33例患者中,12%的患者(4/33)同时出现肌痛(提示肌肉受累)。除了皮肤累及,肺部累及患者10例,可表现为肺部结节伴磨玻璃状影,肺部多发结节伴晕征,肺部浸润,呼吸道粘膜累及,呼吸功能受损,呼吸衰竭等。真菌血症4例。鼻窦累及2例,其中1例表现为鼻窦疼痛,1例表现为鼻窦炎。脑组织累及2例,其中1例表现为纤维性脑膜炎、脑肉芽肿,1例未详细阐述。脓毒性休克1例,为伤口感染引起的骨髓炎导致的脓毒性休克。关节累及1例,表现为关节炎。脾、肾、肝脏等实体器官累及3例。
5 基础病及诱发因素
免疫功能正常的患者皮肤损伤通常是局部的,通常发生在皮肤破裂后,如在创伤、烧伤或已存在的甲癣的部位。在收集的36例患者中,有15例患者的诱发因素为外伤,有3例患者为2型糖尿病,有2位继发于蚊虫叮咬,有2位继发于局部T细胞肿瘤,继发于外用药、慢性丹毒、坏疽性脓皮病、红斑肢痛症、下肢静脉曲张、口腔念珠菌病、肺间质纤维化和粟粒性肺结核等各有1例。
免疫功能受损的患者发生侵袭性镰刀菌病的风险增加,尤其是在长期严重的中性粒细胞减少症和/或严重的细胞免疫缺陷的情况下。与正常宿主的感染不同,免疫缺陷人群中的镰刀菌病具有典型的侵袭性和播散性。在收集的33例免疫缺陷患者中,有24例患者患有血液系统恶性肿瘤的原发疾病,分别为AML(8/33)、ALL(10/33)、非霍奇金淋巴瘤(2/33,其中一例合并HIV)、MDS、AA、MM、急性白血病。有2例器官移植的原发疾病,分别为肾移植、肝移植。其余原发病为STAT1基因错义突变、支气管哮喘、慢性肾功能不全合并糖尿病、复发性骶脊索瘤。诱因可为放化疗后中性粒细胞减少、白细胞功能缺陷、粒细胞功能缺陷、T细胞功能缺陷、甲癣、细菌感染、病毒感染、长期应用糖皮质激素、淤积性皮炎、肺炎、异基因造血干细胞移植等。
6 影像学检查
在收集的患者中,有10例进行了影像学检查,其中有阳性表现的6例,5例为肺部累及,其中4例为血液系统恶性肿瘤患者,CT多表现为双肺多发结节、片状浸润影,也可伴有支气管充气征,胸腔积液等。其中1例为间质性肺疾病合并粟粒性肺结核患者,CT示双肺弥漫性间质改变,纵膈内点状钙化。其中一例骨髓增生异常综合征患者手指被树木刺伤,引起软组织感染肿胀,手部MRI示手指表面及端周软组织增强,掌侧表面可见点状异物(Palmore et al. 2010)。
7 组织病理学
本研究中,在免疫正常的36例患者中,31例患者进行了病理检查,其中26例患者病理中可见真菌结构。皮肤组织苏木精-伊红染色法(hematoxylin-eosin staining,HE)染色可见表皮角化过度、棘层肥厚。真皮内肉芽肿形成,其周围组织伴有慢性炎症细胞散在浸润,小血管内见均匀红染的团块样物质,有细长、分隔、无色菌丝样结构物,过碘雪夫染色法(periodic acid-schiff staining,PAS)染色显示腊肠样菌丝,有分隔及锐角分支,散在卵圆形真菌孢子等。在免疫低下及免疫缺陷的33例患者中,有31例患者采取病理检查,其中25例患者可见真菌结构,病理学检查结果为纤维素样坏死,毛细血管内可见纤维蛋白血栓,经Grocott和PAS染色可见血栓中含有大量菌丝,菌丝与曲霉病和赛多孢子菌病观察到的菌丝相似,约为3-8μm宽,有分隔的透明菌丝,分枝呈两种锐角。急性角状透明分枝分隔菌丝侵犯血管,引起血栓形成和组织梗死。
8 血清学检查
本研究中,其中5例进行了血清学检查,均为免疫低下或免疫缺陷的患者,其中3例患者血清1,3-beta-D-glucan阳性,1例半乳甘露聚糖曲霉抗原检测阳性,1例患者未检测1,3-beta-D-glucan,但半乳甘露聚糖曲霉抗原检测阴性。镰刀菌可释放1,3-beta-D-glucan,但1,3-beta-D-glucan抗原为真菌所共有,不能确定具体菌种,且存在假阳性情况,故其缺乏特异性并不有助于将镰刀菌属确定为侵袭性真菌疾病的病因。1,3-beta-D-glucan在侵袭性镰刀菌病的诊断和监测治疗中的有效性还有待确定。半乳甘露聚糖曲霉抗原检测是侵袭性曲霉病的一种较为特异的检测方法,但镰刀菌属已报道与该检测方法发生交叉反应(Aquino et al. 2007;Tortorano et al. 2012)。因此,高危患者的半乳甘露聚糖阳性试验应被解释为侵袭性曲霉病或侵袭性镰刀菌病的指标,尤其是在侵袭性镰刀菌病较为流行的中心或地区(Nucci et al. 2014)。
9 病原体种类及其药物敏感性
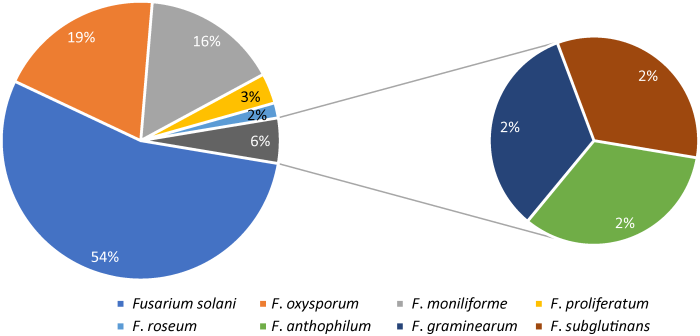
所纳入的69例镰刀菌所致皮肤感染的病例中,全部病例分泌物或组织真菌培养阳性,有54例鉴定到种,16例鉴定到属,共发现8种致病病原体,分别为茄病镰刀菌Fusarium solani、尖孢镰刀菌F. oxysporum、串珠镰刀菌F. moniliforme、层生镰刀菌F. proliferatum、粉红镰刀菌F. roseum、花腐镰刀菌F. anthophilum、禾谷镰刀菌F. graminearum、亚黏团串珠镰刀菌F. subglutinans。所有收集的病例中,茄病镰刀菌F. solani为31例,尖孢镰刀菌F. oxysporum 11例,串珠镰刀菌F. moniliforme 9例,层生镰刀菌F. proliferatum 2例,粉红镰刀菌F. roseum、花腐镰刀菌F. anthophilum、禾谷镰刀菌F. graminearum和亚黏团串珠镰刀菌F. subglutinans各1例,其中有3例患者存在合并感染,分别为茄病镰刀菌F. solani合并尖孢镰刀菌F. oxysporum,串珠镰刀菌F. moniliforme合并茄病镰刀菌F. solani,花腐镰刀菌F. anthophilum合并茄病镰刀菌F. solani(图3)。
图3
大多数镰刀菌分离菌株对两性霉素B敏感。镰刀菌对两性霉素B的敏感性通常高于对唑类(伏立康唑、泊沙康唑和艾沙康唑)的敏感性。如茄病镰刀菌的唑类MIC高于其他镰刀菌种,相比茄病镰刀菌,尖孢镰刀菌与串珠镰刀菌的两性霉素B、伏立康唑及泊沙康唑的MIC较低。某一复合种的敏感性可能随具体种的不同而异。较早的唑类药物,如伊曲康唑、氟康唑、酮康唑的镰刀菌MIC较高。棘白菌素类药物(卡泊芬净、米卡芬净与阿尼芬净)缺乏抗某些镰刀菌种的活性。
10 治疗及预后
在免疫力正常的36例患者中,除8例不详或治疗反复外,其余28例患者经治疗后均取得了改善或愈合。9例患者系统口服伊曲康唑联合局部治疗,2例同时口服两性霉素B。6例患者系统口服酮康唑。4例患者系统口服特比萘芬联合局部治疗,1例患者联合口服异烟肼、利福平等药物,1例患者联合口服伏立康唑及手术治疗。4例患者应用两性霉素B,其中一例为局部注射,另一例合并口服伊曲康唑。辅助手术治疗7例,其中5例合并系统口服药物,2例单纯手术清除病灶。1例患者系统应用氟胞嘧啶,合并其他药物。1例患者单纯外用咪康唑,1例患者系统应用氟康唑,1例患者中药治疗,2例患者辅以局部热疗。
免疫缺陷或免疫低下的33例患者中,有15例患者获得了好转,其中6例患者系统应用两性霉素B和伏立康唑联合治疗,2例患者系统口服伏立康唑,分别辅以中性粒细胞移植、切除排脓治疗。1例单纯手术治疗,1例系统口服酮康唑、氟胞嘧啶联合手术治疗,1例患者系统口服伊曲康唑,1例患者系统口服氟康唑,1例患者系统应用两性霉素B脂质体联合聚烯、外科切除治疗,1例患者系统口服特比萘芬、肌注干扰素治疗,1例患者局部外用氧化锌软膏联合亚醋酸盐2%溶液外用,缓解淤积性皮炎的基础病变后皮疹好转。
11 展望
镰刀菌广泛分布于土壤、植物、及植物碎片等有机质中,也存在于世界范围内的水中(Nelson et al. 1994)。在马铃薯葡萄糖琼脂上,镰刀菌可产生白色、淡紫色、粉红色、鲑鱼色或灰白色菌落,菌落表面呈丝绒状或棉状。微观显微镜下表现为有隔膜的透明菌丝,直径3-8μm,通常分枝锐角。在组织和血液中有形成孢子的能力,因此可观察到游离孢子,类似于酵母菌(Liu et al. 1998)。若同一标本中菌丝和酵母样结构同时出现,则高度提示高危患者患有镰刀菌病。在培养过程中,镰刀菌属可在培养基上产生镰刀形大分生孢子和小分生孢子,大分生孢子为镰刀菌的典型特征外观,常依次进行形态学鉴定,但鉴定至种多较困难,往往需要分子方法(Healy et al. 2005;O′Donnell et al. 2010)。GenBank/EMBL/ DDBJ等国际核酸序列数据库中有关镰刀菌属许多种的ITS序列,所以可通过测定镰刀菌rDNA基因ITS序列来辅助鉴定镰刀菌。rDNA ITS的序列测定、Cfl3 I和Dra II RFLP及种特异性引物用于临床镰刀菌的研究国内缺乏,国外尚不多见(窦红涛等 2008)。使用基质辅助激光解吸/电离飞行时间(MALDI-TOF)质谱法已被证明可以正确地识别临床分离株到种水平(Triest et al. 2015;de Almeida et al. 2016)。
镰刀菌病的诊断依赖于微生物学检查。镰刀菌较容易从皮肤损伤和血液培养中分离出来,皮肤活检组织的培养和直接镜检是确立镰刀菌病最简便易行的方法。由于治疗方法不同,临床常需要鉴别镰刀菌抑或曲霉感染。一般来讲,很难从血液中培养曲霉,镰刀菌病的血培养常常呈阳性。研究资料显示,大约60%的侵袭性镰刀菌病的血液培养呈阳性(Nucci & Anaissie 2007)。其原因可能是由于镰刀菌在体内具有游离孢子,促进了血液中的传播和生长(Liu et al. 1998)。
镰刀菌病的诊断可能需要组织病理学的证实。皮肤活检安全易行,可提供快速诊断。本研究中,90%的患者进行了组织病理学检查,其中82%的患者组织病理中可见真菌结构。由于镰刀菌病与其他霉菌感染在组织学上的相似性,最终的诊断需要在石蜡包埋的组织标本中使用原位杂交或多重实时定量PCR技术进行微生物生长或物种鉴定(Hayden et al. 2003;Salehi et al. 2016)。
镰刀菌病在免疫缺陷或免疫低下患者中最常见的临床表现形式为播散性疾病,研究资料显示,皮肤感染相关的镰刀菌病患者约50%可表现为播散性,表现为长期而持续的中性粒细胞减少,继发皮肤广泛病变(丘疹、结节、坏死性病变),真菌血液培养多阳性。Sampathkumar & Paya(2001)建议将皮肤镰刀菌病分为3组:中央坏死的紫斑结节样病灶、坏疽样脓疮病灶和靶形病灶。其他部位(如原发性或继发性感染)也可被发现,尤其是肺炎、鼻窦炎和肢体蜂窝织炎。在严重中性粒细胞减少症患者中存在难治性发热,伴有多个数量皮肤损伤和血液培养真菌阳性,是提示镰刀菌感染的重要线索。在免疫抑制患者中,虽然播散性镰刀菌感染只占真菌感染的一小部分,但由于其对抗真菌药物具有较强的耐药性,死亡率可达80%-90%(Bushelman et al. 1995;Bodey et al. 2002),临床应给予高度重视。
由于镰刀菌耐药性的存在,镰刀菌病治疗多较为棘手。在免疫力正常的患者中,治疗效果较好。本研究中,系统应用氟康唑、伊曲康唑、氟胞嘧啶、酮康唑、两性霉素B等药物,辅以局部外用咪康唑、手术、热疗均有成功的案例。免疫功能受损的侵袭性镰刀菌病患者需进行积极的抗真菌治疗。研究资料显示,因为不同镰刀菌种对抗真菌药的敏感性各不相同,需要确保给予至少1种有活性的抗真菌药,常联合使用两性霉素B脂质制剂和伏立康唑,也有两种药物单独使用治疗成功的案例。因为镰刀菌几乎总是侵袭免疫功能受损的宿主且常具有散播性,所以应该多方面治疗,对感染组织进行外科清创术或清除受感染的异物也是治疗的重要方法。
抗真菌治疗的剂量和疗程取决于受感染部位和程度、患者的基础疾病与免疫状态、持续免疫抑制的需求,以及对治疗的反应。对于严重免疫功能抑制的患者,抗真菌治疗可能持续数月。抗真菌治疗一般持续到所有感染的体征和症状已消退、放射影像学检查异常的情况已稳定以及已经发生明显的免疫重建。治疗结局中最重要的因素就是中性粒细胞减少症的消退。
由于免疫系统恢复对于镰刀菌病的成功结局至关重要,所以应尽一切努力去增强免疫力。其方法包括可能时减少免疫抑制药物的剂量和使用辅助免疫疗法,例如粒细胞集落刺激因子(granulocyte colony-stimulating factor,G-CSF)或粒-巨噬细胞集落刺激因子(granulocyte- macrophage colony-stimulating factor,GM-CSF)、G-CSF-刺激的粒细胞输注、G-CSF联用地塞米松-刺激的粒细胞输注,或者干扰素γ辅助治疗。这些疗法对于镰刀菌病的有效性还未确定(Hennequin et al. 1994;Dignani et al. 1997)。其他的治疗策略包括对感染组织(如鼻窦、软组织、肺结节)进行外科清创术(Kadri et al. 2015),尤其是有局灶性疾病的免疫功能受损患者,以及对疑诊导管相关的镰刀菌病患者拔除中心静脉导管(Lupinetti et al. 1990)。
总之,镰刀菌病在世界各地均有报道,免疫正常及免疫低下患者均可患病,免疫正常感染多为局限性,免疫低下患者感染多表现为播散性。镰刀菌存在多重耐药状况,建议临床进行药敏测定,并以联合用药治疗。
参考文献
Fusarium meningoencephalitis in a child with acute leukemia
DOI:10.1055/s-2008-1071428
URL
PMID:1857495

A 15-year-old boy with acute lymphoblastic leukemia (ALL) developed disseminated fusarium infection with meningoencephalitis following a contaminated skin wound. With antifungal therapy, the cutaneous lesions cleared but central nervous system (CNS) infection persisted causing a fibrosing meningitis and a brain granuloma. Fusaria are soil saprophytes that are more commonly associated with superficial eye and skin lesions, but may also cause severe systemic infections with CNS involvement in immuno-compromised patients. The organism may be confused with Aspergillus in tissue sections, and can only be diagnosed by culture.
Antifungal susceptibil ity profile of clinical Fusarium spp. isolates identified by molecular methods
DOI:10.1093/jac/dkn022
URL
PMID:18263569
[本文引用: 1]

OBJECTIVES: To analyse the susceptibility pattern of a collection of Fusarium clinical isolates. METHODS: The antifungal susceptibility pattern of 67 isolates of Fusarium was analysed. Strains were identified by morphological and molecular methods by means of sequencing elongation factor alpha. RESULTS AND CONCLUSIONS: Six different species were identified. Fusarium solani was the most frequently isolated, followed by Fusarium oxysporum, Fusarium proliferatum and Fusarium verticilloides. Amphotericin B was the only drug with in vitro activity (range: 0.015-32 mg/L). The rest of the antifungals tested (itraconazole, voriconazole, ravuconazole, posaconazole and terbinafine) showed very poor activity against Fusarium, confirming the multiresistant nature of this genus.
Update on the contribution of galactomannan for the diagnosis of invasive aspergillosis
DOI:10.1007/s11046-007-9010-2
URL
[本文引用: 1]

The diagnosis of invasive fungal infections (IFI) remains a challenge, particularly for diseases caused by filamentous fungi such as Aspergillus species. Unfortunately, many patients affected by these conditions are not identified before autopsy. Therefore, there is a need for new diagnostic methods for IFI. Galactomannan is a soluble antigen released during hyphal growth in tissues. A commercially available sandwich ELISA assay that detects galactomannan has been used in Europe for many years and is now approved for use in the USA. The test has an excellent negative predictive value in the detection of invasive aspergillosis (IA) in high-risk patients. In addition, it is more sensitive than culture and allows IA to be diagnosed before clinical manifestations occur. However, false-negative and false-positive results in certain populations are the main limitations to its use. The purpose of this review is to summarize the current knowledge about galactomannan testing in patients at risk for IA.
Extensive subcutaneous hyphomycosis caused by Fusarium oxysporum
Subcutaneous granulomatous lesions by hyaline moulds are rare. This report describes a case of hyalohyphomycosis by Fusarium oxysporum. The patient was a 16-year-old Sri Lankan girl who had had extensive lesions in both arms almost from infancy. The fungus was demonstrated in KOH mounts and in histopathological sections. It was isolated repeatedly from her lesions over a period of 10 months. Combined therapy with ketoconazole and 5-fluorocytosine resulted in marked improvement. An inherent immune defect is postulated to account for the prolonged and extensive infection by a relatively non-aggressive fungus.
Sequence-based identification of Aspergillus, Fusarium, and Mucorales species in the clinical mycology laboratory: where are we and where should we go from here?
DOI:10.1128/JCM.01685-08 URL PMID:19073865 [本文引用: 1]
Mycetoma of the foot due to Fusarium sp. treated with oral ketoconazole
DOI:10.1159/000247578
URL
PMID:1498403

We report the case of a 30-year-old Nigerian patient with mycetoma of the foot without bone involvement caused by Fusarium sp..Long-term administration of ketoconazole produced a significant improvement with good clinical and biological tolerance.
Facial granuloma associated with Fusarium infection
Skin lesions associated with Fusarium infection
DOI:10.1067/mjd.2002.123489
URL
PMID:12399756
[本文引用: 1]

Infections caused by Fusarium species are increasing in frequency among immunocompromised hosts. We identified 35 patients with cancer who had Fusarium skin lesions. Twenty patients had disseminated infection, 6 had primary localized skin infections, 4 had skin lesions associated with sinus infections, and 5 had onychomycosis. All patients (except 3 with onychomycosis) had hematologic malignancies and neutropenia. Skin lesions associated with disseminated infection included red or gray macules, papules (some with central necrosis or eschar), pustules, and subcutaneous nodules. Most patients had a variety of lesions simultaneously. Multiple red or gray macules with central ulceration or black eschar are characteristic of Fusarium infection. Disseminated infection may originate from skin lesions or onychomycosis. Most infections fail to respond to antifungal therapy unless there is resolution of the patient's neutropenia.
Clinicopathologic challenge. Disseminated fusariosis
DOI:10.1111/j.1365-4632.2007.03332.x URL PMID:18173593
Disseminated Fusarium solani infection
DOI:10.1016/0190-9622(95)90401-8
URL
PMID:7829738
[本文引用: 1]

Disseminated fungal infections commonly occur in immunocompromised hosts; Candida spp. are the most common. Fusarium spp., soil saprophytes once considered pathogenic only in plants, have emerged as serious pathogens in neutropenic patients with malignancies. We describe two patients, one with acute myelogenous leukemia and the other with metastatic breast cancer, in whom disseminated Fusarium solani infection developed. Both patients had neutropenia and fever when generalized, tender, erythematous papules developed; most of the papules had black necrotic centers. Despite aggressive therapy with antifungal agents and granulocyte-macrophage colony-stimulating factor, both patients died within 1 month. Disseminated Fusarium infection can be a life-threatening condition in which skin lesions are frequently the initial sign. Early recognition and hematopoietic recovery offer the best chance for survival.
Post traumatic subcutaneous mycosis due to Fusarium solani
One case of infantile facial Fusarium infection
Foot hyalohyphomycosis caused by Fusarium subglutinans: a case report
Cutaneous infection in man caused by Fusarium moniliforme
Fusarium moniliforme was isolated from a pustular lesion on the hand of an otherwise healthy male. Branching hyphae were seen in pus stained by the periodic acid-Schiff method. Pustular lesions containing branching hyphae were produced in mice after subcutaneous injection of microconidia. The experimental infection in mice and the naturally occurring lesion in man healed without treatment in 1 to 2 weeks. Although production of catenulate microconida was abundant on several common laboratory media, the characteristic macroconidia of F. moniliforme were produced only on barley-pea-rice straw agar.
Rapid identification of moulds and arthroconidial yeasts from positive blood cultures by MALDI-TOF mass spectrometry
DOI:10.1093/mmy/myw044
URL
PMID:27317582
[本文引用: 1]

Moulds and arthroconidial yeasts are potential life-threatening agents of fungemia in immunocompromised patients. Fast and accurate identification (ID) of these pathogens hastens initiation of targeted antifungal therapy, thereby improving the patients' prognosis. We describe a new strategy that enabled the identification of moulds and arthroconidial yeasts directly from positive blood cultures by MALDI-TOF mass spectrometry (MS). Positive blood cultures (BCs) with Gram staining showing hyphae and/or arthroconidia were prospectively selected and submitted to an in-house protein extraction protocol. Mass spectra were obtained by Vitek MS system, and identifications were carried out with in the research use only (RUO) mode with an extended database (SARAMIS [v.4.12] plus in-house database). Fusarium solani, Fusarium verticillioides, Exophiala dermatitidis, Saprochaete clavata, and Trichosporon asahii had correct species ID by MALDI-TOF MS analysis of positive BCs. All cases were related to critically ill patients with high mortality fungemia and direct ID from positive BCs was helpful for rapid administration of targeted antifungal therapy.
Treatment of neutropenia-related fungal infections with granulocyte colony-stimulating factor-elicited white blood cell transfusions: a pilot study
DOI:10.1038/sj.leu.2400811
URL
PMID:9324280
[本文引用: 1]

Neutropenia-related fungal infections can be life-threatening despite antifungal therapy. We evaluated the role of recombinant granulocyte colony-stimulating factor (rG-CSF)-elicited white blood cell (WBC) transfusions in patients with neutropenia-related fungal infections. Adult patients with hematologic malignancies, absolute neutrophil counts (ANC) <500/microl and fungal infections refractory to amphotericin B, received daily transfusions of rG-CSF-elicited and irradiated WBC transfusions from related donors. Donors received 5 microg/kg/day of rG-CSF subcutaneously. Donors achieved a mean ANC of 29.4 x 10(3) per microliter. The mean yield of neutrophils per transfusion was 41 x 10(9) (range, 10-116). Fifteen patients received a median of eight transfusions (range, 3-16). Fourteen patients had received rG-CSF for a median of 12 days. The median ANC baseline was 20/microl. Eleven patients had favorable responses and eight of them remained free of infection 3 weeks after therapy. Favorable responses occurred among patients with better Zubrod performance status (median, 3 vs 4) and shorter duration of both profound neutropenia (median, 15 vs 25 days) and active infection (median, 8 vs 17 days). The mean 1- and 24-h post-transfusion ANCs were 594/microl (range, 98-1472/microl) and 396/microl (range, 50-1475/microl), respectively. Adverse reactions were observed in nine of 35 donors and in the recipients of six of 130 transfusions. rG-CSF-elicited WBC transfusions may be a safe and promising approach for treating neutropenia-related fungal infections.
Fusariosis in a patient with acute myeloid leukemia: a case report and review of the literature
DOI:10.1007/s11046-016-9987-5
URL
PMID:27008433

Fusarium spp. causes infections mostly in patients with prolonged neutropenia. We describe the case of a disseminated Fusarium solani infection in a patient with acute myeloid leukemia which never reached complete remission during its clinical course. The patient had profound neutropenia and developed skin nodules and pneumonia in spite of posaconazole prophylaxis. F. solani was isolated from blood and skin biopsy, being identified from its morphology and by molecular methods. By broth dilution method, the strain was resistant to azoles, including voriconazole and posaconazole, and to echinocandins. MIC to amphotericin B was 4 mg/L. The patient initially seemed to benefit from therapy with voriconazole and amphotericin B, but, neutropenia perduring, his clinical condition deteriorated with fatal outcome. All efforts should be made to determine the correct diagnosis as soon as possible in a neutropenic patient and to treat this infection in a timely way, assuming pathogen susceptibility while tests of antimicrobial susceptibility are pending. A review of the most recent literature on invasive fungal infections is reported.
Identification of clinically important Fusarium spp
Mixed infection caused by two species of Fusarium in a human immunodeficiency virus-positive patient
DOI:10.1128/JCM.38.9.3460-3462.2000
URL
PMID:10970404

We report on a case of mixed infection caused by two species of Fusarium in a human immunodeficiency virus-positive patient with lymphoma who was neutropenic due to chemotherapy. The patient showed the typical signs of a disseminated fusarial infection, with Fusarium solani isolated from skin lesions and F. verticillioides isolated from blood. The report discusses how difficult it is to make an accurate diagnosis when an immunosuppressed patient is infected with more than one fungal species, especially when the species are morphologically very similar.
One case of hyalohyphomycosis in the foot due to Fusarium solani
One patient was diagnosed as hyalohyphomycosis by history,medical examnation,pathology and fungal culture.The pathogen was finally identified as Fusarium solani.The patient showed significant improvement after 3-month treatment with itraconazole and part-leision resection.
Cellulitis and nodular skin lesions due to Fusarium spp. in liver transplant: case report
Disseminated fusariosis with cutaneous involvement in hematologic malignancies: report of six cases with high mortality rate
DOI:10.1590/abd1806-4841.20187476
URL
PMID:30156626

Fusariosis is due to inhalation or direct contact with conidia. Clinical presentation depends on host's immunity and can be localized, focally invasive or disseminated. Given the severity of this infection and the possibility for the dermatologist to make an early diagnosis, we report six cases of patients with hematologic malignancies, who developed febrile neutropenia an skin lesions suggestive of cutaneous fusariosis. All patients had skin cultures showing growth of Fusarium solani complex, and they received amphotericin B and voriconazole. As this infection can quickly lead to death, dermatologists play a crucial role in diagnosing this disease.
In situ hybridization for the differentiation of Aspergillus, Fusarium, and Pseudallescheria species in tissue section
DOI:10.1097/00019606-200303000-00003
URL
PMID:12605032
[本文引用: 1]

Identification of fungi in tissue sections can be difficult. In particular, species of Aspergillus, Fusarium, and Pseudallescheria all appear as septate, branched hyphae. However, their differentiation can have significant clinical implications, as the latter two groups are often resistant to commonly used antifungal agents. In situ hybridization may assist in rapidly distinguishing these organisms in the absence of available culture. Oligonucleotide DNA probes were directed against the 5S, 18S, or 28S rRNA sequences of three groups of fungi with a high degree of specificity for each. Probes were tested on 26 formalin-fixed, paraffin-embedded tissue specimens, each with culture-proven involvement by one of these organisms: Fusarium species, n = 12; Pseudallescheria boydii, n = 5; Aspergillus species, n = 9 ( probe set validated in an earlier study). Accuracy of both ISH and morphology was compared with culture. Morphologic examination (GMS and PAS) showed a greater sensitivity in detecting fungi (100%) as compared with in situ hybridization (84.6%). When detected, however, DNA probes allowed definitive identification of organisms. While there was no ability to distinguish between the three groups of organisms by morphologic features, ISH probes showed 100% positive predictive value (PPV, 19/19 organisms identified correctly). No cross-reactivity was observed when the probes were tested against other genera (100% specificity). Furthermore, the use of ISH allowed the detection of mixed fungal infections involving multiple organism types in two cases, demonstrating another advantage over morphology. In situ hybridization, directed against rRNA sequences, provides a rapid and accurate technique for distinguishing commonly encountered, nonpigmented filamentous fungi in histologic sections. While less sensitive than morphology, ISH is highly accurate and may help to distinguish between organisms that have similar or identical morphologic features by light microscopy.
Use of the diversi lab system for species and strain differentiation of Fusarium species isolates
DOI:10.1128/JCM.43.10.5278-5280.2005
URL
PMID:16207996
[本文引用: 1]

Advances in molecular typing of fusariosis would facilitate the study of its epidemiology. We tested 26 such isolates by the commercially available Diversi Lab System. The system utilizes automated repetitive sequence-based PCR (rep-PCR) and web-based data analyses. rep-PCR dendrogram cluster analysis showed agreement with species sequence identification (elongation factor 1 alpha gene). Additionally, subtype differences within the same species were noted.
Role of granulocyte colony-stimulating factor in the management of infection with Fusarium oxysporum in a neutropenic child
DOI:10.1093/clinids/18.3.490 URL PMID:7516720 [本文引用: 1]
Invasive fusariosis associated with an injury by a stingray barb
Fusarium solani infection in a patient after allogeneic hemotopoietic stem cell transplantation:case report and literature review
Objective To study Fusarium solani infection as a complication in patients after allogeneic hemotopoietic stem cell transplantation and to discuss the diagnosis and appropriate therapy.Methods Symptoms, physical examination, laboratory tests, computed tom
A case of cutaneous hyalohyphomycosis caused by Fusarium solani
Fusarium septicaemia happened in children with acute lymphoblastic leukemia
One case of leg ulcer caused by Fusarium moniliforme
Role of granulocyte transfusions in invasive fusariosis: systematic review and single-center experience
DOI:10.1111/trf.13099
URL
PMID:25857209
[本文引用: 1]

BACKGROUND: Invasive Fusarium infection is relatively refractory to available antifungal agents. Invasive fusariosis (IF) occurs almost exclusively in the setting of profound neutropenia and/or systemic corticosteroid use. Treatment guidelines for IF are not well established, including the role of granulocyte transfusions (GTs) to counter neutropenia. STUDY DESIGN AND METHODS: We conducted a systematic review, identifying IF cases where GTs were used as adjunctive therapy to antifungal agents and also report a single-center case series detailing our experience (1996-2012) of all IF cases treated with antifungal agents and GTs. In the systematic review cases, GTs were predominantly collected from nonstimulated donors whereas, in the case series, they were universally derived from dexamethasone- and granulocyte-colony-stimulating factor-stimulated donors. RESULTS: Twenty-three patients met inclusion criteria for the systematic review and 11 for the case series. Response rates after GTs were 30 and 91% in the review and case series, respectively. Survival to hospital discharge remained low at 30 and 45%, respectively. Ten patients in the systematic review and three in the case series failed to achieve hematopoietic recovery and none of these survived. In the case series, donor-stimulated GTs generated mean
Intra-articular injection of voriconazole for Fusarium solani arthritis after bone marrow transplantation
DOI:10.1016/j.jinf.2012.06.001 URL PMID:22705652
Subcutaneous hyalohyphomycosis caused by Fusarium in a kidney transplant recipient
DOI:10.3109/0886022X.2014.926756
URL

Fusarium is a filamentous opportunistic pathogenic fungus responsible for superficial as well as invasive infection in immunocompromized hosts. Net state of immunosuppression and cytomegalovirus (CMV) infection appear to predispose to this disease which is life-threatening when disseminated. Though infections with Fusarium have been widely described in hematological malignancies and hematopoietic stem cell transplant cases, they have been reported to be rare in solid organ transplant recipients, are often localized and carry a favorable prognosis. We here describe a rare case of subcutaneous non-invasive infection with Fusarium in a renal allograft recipient two and half years after transplantation. Patient had a previous history of CMV infection along with multiple other recurrent co-infections. Diagnosis was based on culture of tissue specimens yielding Fusarium species. The infection had a protracted course with persistence of lesions after treatment with voriconazole alone, requiring a combination of complete surgical excision and therapy with the anti-fungal drug.
Successful treatment of disseminated fusariosis with voriconazole in an acute lymphoblastic leukaemia patient
DOI:10.1111/myc.2011.54.issue-s4 URL
Systemic ketoconazole treatment for Fusarium leg ulcers
DOI:10.1111/j.1365-4362.1992.tb02705.x
URL
PMID:1500248

Fusarium oxysporum was isolated from a large foot ulcer in an otherwise healthy 69-year-old man. Although tissue invasion could not be proven histologically, systemic antifungal treatment was administered with satisfactory response. Fusarium species are common soil-inhabiting organisms and plant pathogens. In humans, Fusarium is considered an opportunistic agent in skin ulcers, interdigital spaces, and burned skin, but can also cause mycotic keratitis, onychomycosis, and rarely deep-seated or disseminated infections, especially in an immunocompromised host. The distinction between skin infection and saprophytic growth, as well as optimal treatment regimens for the two types of infection, have not been clearly defined. We describe a case of leg ulcers caused by Fusarium oxysporum in a 69-year-old man treated successfully with oral ketoconazole.
Recurrence of Fusarium solani abscess formation in an otherwise healthy patient
DOI:10.1007/BF01716292
URL
PMID:8557391

Fusarium spp. are usually considered opportunistic fungi in humans. A case of Fusarium solani abscess formation of the foot in an immunocompetent patient in whom recurrence occurred even after intravenous amphotericin B treatment is presented here.
One case of Fusarium oxysporum infection secondary to erythromelalgia
Foot ulcer caused by Fusarium solani: a case report
Morphologic criteria for the preliminary identification of Fusarium, Paecilomyces, and Acremonium species by histopathology
DOI:10.1093/ajcp/109.1.45
URL
PMID:9426517
[本文引用: 2]

Nontraditional human pathogenic fungi, including Fusarium, Paecilomyces, and Acremonium species, have been increasingly documented as agents of infection in immunocompromised patients and, occasionally, in normal hosts. Although definitive identification of these fungi requires culture, they often can be identified provisionally in tissue sections by a combination of histologic features, including hyaline septate hyphae and characteristic reproductive structures known as phialides and phialoconidia. These morphologic characteristics, although familiar to mycologists, are easily overlooked by histopathologists; as a result, Fusarium species and Paecilomyces lilacinus are frequently misidentified in tissue sections as Aspergillus or Candida species. We identified 19 culture-proved cases of infection with species of Fusarium, Paecilomyces, or Acremonium; retrospectively reviewed histologic specimens stained by routine hematoxylin and eosin, Gomori methenamine silver, and/or periodic acid-Schiff stains; and delineated morphologic criteria that will help pathologists make a preliminary identification of these fungi by histopathology. Adventitious sporulation was found in 9 of 9 infections caused by Paecilomyces species, 7 of 10 infections caused by Fusarium species, and in the single case of infection caused by Acremonium strictum. Histologic recognition of these morphologies may help clinicians select appropriate initial antifungal treatment and manage the infection.
A case of cutaneous hyalohyphomycosis caused by Fusarium solani
Operative treatment of Fusarium fungal infection of the lung
DOI:10.1016/0003-4975(90)90885-a
URL
PMID:2369203
[本文引用: 1]

Systemic fungal infections with Fusarium occur predominantly in immunocompromised patients and are usually fatal. We report a patient with acute lymphocytic leukemia and fusariosis involving the skin and lungs. This patient underwent antifungal chemotherapy and bilateral pulmonary resections. She subsequently had successful bone marrow transplantation. The results of this treatment suggest that this aggressive management of pulmonary fusariosis offers the best chance of survival.
Cutaneous Fusarium moniliforme infection in a child
Fusarium oxysporum infection of stasis ulcer: eradication with measures aimed to improve stasis
DOI:10.1111/j.1439-0507.2009.01800.x
URL
PMID:19878456

Fusarium species may cause localised skin infections in immunocompetent individuals. At least half of these infections are preceded by skin breakdown. The lesions are characterised by slow progression and good response to therapy. Here we present a 60-year-old non-diabetic man with stasis ulcers showing Fusarium oxysporum growth in culture of both pus swabs and skin biopsy specimens. The patient was confined to wheelchair because of recurrent sacral chordoma of 15 years duration, which was not under treatment for the last 3 years. Leg ulcers were resistant to antifungal therapy, and healed rapidly after improving of stasis with local and systemic measures.
Transepidermal growth in disseminated Fusarium infection
Deep cutaneous infection by Fusarium solani in a healthy child: successful treatment with local heat therapy
DOI:10.1016/j.jaad.2006.10.960
URL

We describe a 6-year-old boy with a granulomatous lesion on the upper aspect of his left arm. Fusarium solani infection was confirmed by biopsy studies and cultures. The biopsy specimen showed an unusually extensive dermal invasion with fungal hyphae. This is an uncommon clinical presentation for deep cutaneous infection caused by F solani in a healthy child. Local heat therapy with a chemical pocket warmer led to dramatic healing of the lesion.
A cutaneous ulcer induced by fungi of the genus Fusarium
DOI:10.1590/s0037-86821997000400008
URL
PMID:9265228

A case of cutaneous hyalohyphomycosis, due to Fusarium oxysporum, in a 40 years old man is presented. The patient came from Paraguay where he worked in a tropical rural area. His disease had begun 2 months before his admission as a skin ulcer located in the left leg. Clinical characteristics, diagnosis methods, differential diagnosis with other ulcers of the legs in tropical areas as well as therapeutic measures are discussed in this presentation.
Taxonomy, biology, and clinical aspects of Fusarium species
DOI:10.1128/cmr.7.4.479
URL
PMID:7834602
[本文引用: 1]

There are several taxonomic systems available for identifying Fusarium species. The philosophy used in each taxonomic system is discussed as well as problems encountered in working with Fusarium species in culture. Fusarium species are toxigenic, and the mycotoxins produced by these organisms are often associated with animal and human diseases. The implications for the association of the carcinogens, fumonisins, produced by Fusarium moniliforme and other Fusarium species with human diseases are discussed. Foreign-body-associated fusarial infection such as keratitis in contact lens wearers, onychomycosis, skin infections, and disseminated multiorgan infections are discussed. Disseminated fusarial hyalohyphomycosis has emerged as a significant, usually fatal infection in the immunocompromised host. Successful outcome is determined by the degree of immunosuppression, the extent of the infection, and the presence of a removable focus such as an indwelling central venous catheter. These infections may be clinically suspected on the basis of a constellation of clinical and laboratory findings, which should lead to prompt therapy, probably with one of the newer antifungal agents. Perhaps the use of such agents or the use of colony-stimulating factors may improve the outcome of this devastating infection. However, until new approaches for treatment develop, effective preventive measures are urgently needed.
Fusarium infections in immunocompromised patients
DOI:10.1128/CMR.00014-07
URL
PMID:17934079
[本文引用: 2]

Fusarium species cause a broad spectrum of infections in humans, including superficial, locally invasive, and disseminated infections. The clinical form of fusariosis depends largely on the immune status of the host and the portal of entry, with superficial and localized disease occurring mostly in immunocompetent patients and invasive and disseminated disease affecting immunocompromised patients. Risk factors for severe fusariosis include prolonged neutropenia and T-cell immunodeficiency, especially in hematopoietic stem cell transplant recipients with severe graft-versus-host disease. The most frequent presentation of disseminated fusariosis is a combination of characteristic cutaneous lesions and positive blood cultures, with or without lung or sinus involvement. The prognosis is poor and is determined largely by degree of immunosuppression and extent of infection, with virtually a 100% death rate among persistently neutropenic patients with disseminated disease. These infections may be clinically suspected on the basis of a constellation of clinical and laboratory findings, which should lead to prompt therapy. Treatment options include the lipid formulations of amphotericin B, voriconazole, and posaconazole. Prevention of fusarial infection among high-risk patients should be considered.
Earlier diagnosis of invasive fusariosis with Aspergillus serum galactomannan testing
DOI:10.1371/journal.pone.0087784
URL
PMID:24489964
[本文引用: 1]

Cross-reactivity of Fusarium species with serum galactomannan antigen (GMI) test has been observed. We sought to evaluate if GMI could help to early diagnose invasive fusariosis and to monitor treatment response. We reviewed the records of all patients with invasive fusariosis between 2008 and 2012 in three Brazilian hospitals. We selected patients who had at least 1 GMI test within 2 days before or after the date of the first clinical manifestation of fusariosis, and analyzed the temporal relationship between the first positive GMI test and the date of the diagnosis of invasive fusariosis, and the kinetics of GMI in relation to patients' response to treatment. We also selected 18 controls to determine the sensitivity and specificity of the test. Among 18 patients, 15 (83%) had at least one positive GMI (median 4, range 1-15). The sensitivity and specificity of was 83% and 67%, respectively. GMI was positive before the diagnosis of invasive fusariosis in 11 of the 15 cases (73%), at a median of 10 days (range 3-39), and after the diagnosis in 4 cases. GMI became negative in 8 of the 15 patients; 3 of these 8 patients (37.5%) were alive 90 days after the diagnosis of fusariosis compared with 2 of 7 (29%) who did not normalize GMI (p = 1.0). GMI is frequently positive in invasive fusariosis, and becomes positive before diagnosis in most patients. These findings may have important implications for the choice of antifungal therapy in settings with high prevalence of invasive fusariosis.
Beta-D-glucan as a diagnostic adjunct for invasive fungal infections: validation, cutoff development, and performance in patients with acute myelogenous leukemia and myelodysplastic syndrome
DOI:10.1086/421944
URL
PMID:15307029

The Glucatell (1-->3)- beta-D-glucan (BG) detection assay (Associates of Cape Cod) was studied as a diagnostic adjunct for invasive fungal infections (IFIs). On the basis of findings from a preliminary study of 30 candidemic subjects and 30 healthy adults, a serum BG level of >or=60 pg/mL was chosen as the cutoff. Testing was performed with serial serum samples obtained from 283 subjects with acute myeloid leukemia or myelodysplastic syndrome who were receiving antifungal prophylaxis. At least 1 serum sample was positive for BG at a median of 10 days before the clinical diagnosis in 100% of subjects with a proven or probable IFI. IFIs included candidiasis, fusariosis, trichosporonosis, and aspergillosis. Absence of a positive BG finding had a 100% negative predictive value, and the specificity of the test was 90% for a single positive test result and >or=96% for >or=2 sequential positive results. The Glucatell serum BG detection assay is highly sensitive and specific as a diagnostic adjunct for IFI.
Molecular phylogenetic diversity, multilocus haplotype nomenclature, and in vitro antifungal resistance within the Fusarium solani species complex
DOI:10.1128/JCM.02371-07
URL
PMID:18524963
[本文引用: 1]

Members of the species-rich Fusarium solani species complex (FSSC) are responsible for approximately two-thirds all fusarioses of humans and other animals. In addition, many economically important phytopathogenic species are nested within this complex. Due to their increasing clinical relevance and because most of the human pathogenic and plant pathogenic FSSC lack Latin binomials, we have extended the multilocus haplotype nomenclatural system introduced in a previous study (D. C. Chang, G. B. Grant, K. O'Donnell, K. A. Wannemuehler, J. Noble-Wang, C. Y. Rao, L. M. Jacobson, C. S. Crowell, R. S. Sneed, F. M. T. Lewis, J. K. Schaffzin, M. A. Kainer, C. A. Genese, E. C. Alfonso, D. B. Jones, A. Srinivasan, S. K. Fridkin, and B. J. Park, JAMA 296:953-963, 2006) to all 34 species within the medically important FSSC clade 3 to facilitate global epidemiological studies. The typing scheme is based on polymorphisms in portions of the following three genes: the internal transcribed spacer region and domains D1 plus D2 of the nuclear large-subunit rRNA, the translation elongation factor 1 alpha gene (EF-1alpha), and the second largest subunit of RNA polymerase II gene (RPB2). Of the 251 isolates subjected to multilocus DNA sequence typing, 191 sequence types were differentiated, and these were distributed among three strongly supported clades designated 1, 2, and 3. All of the mycosis-associated isolates were restricted to FSSC clade 3, as previously reported (N. Zhang, K. O'Donnell, D. A. Sutton, F. A Nalim, R. C. Summerbell, A. A. Padhye, and D. M. Geiser, J. Clin. Microbiol. 44:2186-2190, 2006), and these represent at least 20 phylogenetically distinct species. Analyses of the combined DNA sequence data by use of two separate phylogenetic methods yielded the most robust hypothesis of evolutionary relationships and genetic diversity within the FSSC to date. The in vitro activities of 10 antifungals tested against 19 isolates representing 18 species that span the breadth of the FSSC phylogeny show that members of this complex are broadly resistant to these drugs.
Internet-accessible DNA sequence database for identifying fusaria from human and animal infections
DOI:10.1128/JCM.00989-10
URL
PMID:20686083
[本文引用: 1]

Because less than one-third of clinically relevant fusaria can be accurately identified to species level using phenotypic data (i.e., morphological species recognition), we constructed a three-locus DNA sequence database to facilitate molecular identification of the 69 Fusarium species associated with human or animal mycoses encountered in clinical microbiology laboratories. The database comprises partial sequences from three nuclear genes: translation elongation factor 1alpha (EF-1alpha), the largest subunit of RNA polymerase (RPB1), and the second largest subunit of RNA polymerase (RPB2). These three gene fragments can be amplified by PCR and sequenced using primers that are conserved across the phylogenetic breadth of Fusarium. Phylogenetic analyses of the combined data set reveal that, with the exception of two monotypic lineages, all clinically relevant fusaria are nested in one of eight variously sized and strongly supported species complexes. The monophyletic lineages have been named informally to facilitate communication of an isolate's clade membership and genetic diversity. To identify isolates to the species included within the database, partial DNA sequence data from one or more of the three genes can be used as a BLAST query against the database which is Web accessible at FUSARIUM-ID (http://isolate.fusariumdb.org) and the Centraalbureau voor Schimmelcultures (CBS-KNAW) Fungal Biodiversity Center (http://www.cbs.knaw.nl/fusarium). Alternatively, isolates can be identified via phylogenetic analysis by adding sequences of unknowns to the DNA sequence alignment, which can be downloaded from the two aforementioned websites. The utility of this database should increase significantly as members of the clinical microbiology community deposit in internationally accessible culture collections (e.g., CBS-KNAW or the Fusarium Research Center) cultures of novel mycosis-associated fusaria, along with associated, corrected sequence chromatograms and data, so that the sequence results can be verified and isolates are made available for future study.
Disseminated cutaneous Fusarium infection with vascular invasion in a leukemic patient. Journal of Medical and Veterinary Mycology: Bi-monthly Publication of the International Society for Human and
Granuloma annulare-like skin lesion due to Fusarium roseum: therapy with ketoconazole
Multicenter clinical evaluation of the (1-->3) beta-D-glucan assay as an aid to diagnosis of fungal infections in humans
DOI:10.1086/432470
URL
PMID:16080087

BACKGROUND: Measurement of (1-->3)-beta-D-Glucan (BG) has emerged as an adjunct diagnostic strategy for invasive fungal infections (IFI). METHODS: Subjects at 6 clinical sites in the United States were enrolled as either fungal infection-negative subjects (n = 170) or subjects with proven or probable IFI according to European Organization for the Research and Treatment of Cancer/Mycoses Study Group criteria (n = 163). A central laboratory and 4 sites performed assays. A single sample was obtained per patient and was evaluated using an assay to detect serum BG derived from fungal cell walls (range, 0 to > 7000 pg/mL). RESULTS: At a cutoff of 60 pg/mL, the sensitivity and specificity of the assay were 69.9% and 87.1%, respectively, with a positive predictive value (PPV) of 83.8% and a negative predictive value (NPV) of 75.1%. At a cutoff value of 80 pg/mL, the sensitivity and specificity were 64.4% and 92.4%, respectively, with a PPV of 89% and an NPV of 73%. Of the 107 patients with proven candidiasis, 81.3% had positive results at a cutoff value of 60 pg/mL, and 77.6% had positive results at a cutoff value of 80 pg/mL. Of the 10 patients with aspergillosis, 80% had positive results at cutoff values of 60 and 80 pg/mL. The 3 subjects diagnosed with Fusarium species had positive results at a cutoff value of 60 pg/mL. Patients infected with Mucor or Rhizopus species (both of which lack BG) had negative results at both cutoff values, and of the 12 patients with Cryptococcus infection, 3 had positive results at a cutoff value of 60 pg/mL, and 2 had positive results at a cutoff value of 80 pg/mL. Of the subjects with proven positive results who were receiving antifungal therapy (n = 118), 72.9% had results positive for BG at a cutoff value of 60 pg/mL, and 69.5% had results positive for BG at a cutoff value of 80 pg/mL. The interlaboratory sample test r2 was 0.93. CONCLUSION: Reproducible assay results with high specificity and high PPV in a multicenter setting demonstrate that use of an assay to detect serum BG derived from fungal cell walls is a useful diagnostic adjunct for IFI.
Fusarium proliferatum soft tissue infection at the site of a puncture by a plant: recovery, isolation, and direct molecular identification
DOI:10.1128/JCM.01525-09
URL
PMID:19923491
[本文引用: 1]

After allogeneic stem cell transplantation, a 49-year-old man developed fever and inflammation at the site of a plant puncture on a finger. A hyalohyphomycete was recovered by incubating the plant spine fragment following surgery. Amplification of the internal transcribed spacer region and 5.8S rRNA, beta-tubulin, and translation elongation factor coding genes identified Fusarium proliferatum, which was confirmed later by culture.
Case report. Pathohistological findings in a clinical case of disseminated infection with Fusarium oxysporum
DOI:10.1046/j.1439-0507.2000.00590.x
URL
PMID:11105540

Despite appropriate antimicrobial and antifungal therapy (amphotericin B), a disseminated infection with Fusarium oxysporum in a 75-year-old immunocompromised patient (acute myeloid leukaemia, minimal leucocyte count of 0.5 giga l-1) led rapidly to death. A similarly fatal course of an F. oxysporum infection has been reported in several cases. Fusarium oxysporum could be isolated shortly before death from blood cultures and from a swab taken from skin efflorescences. An autopsy revealed histopathologically typical fungal infiltrates in the mucosa of the pharynx, epiglottis, trachea, and oesophagus and in the parenchyma of the spleen, the lung and both kidneys. Because of the high risk of a fatal outcome of this infection, the clinician should aim at maximum diagnostic enforcement. We propose both analysis of blood cultures and immediate skin biopsy--with PAS-staining--of suspicious dermal efflorescences for microscopic examination. The treatment of choice is discussed controversially but a beneficial effect has been reported from granulocyte transfusion, subcutaneous administration of GM-CSF and concomitant treatment with amphotericin B.
Chronic infection due to Fusarium oxysporum mimicking lupus vulgaris: case report and review of cutaneous involvement in fusariosis
DOI:10.1080/000155501750208218
URL
PMID:11411917

A 67-year-old female presented with a 20-year-old lesion involving the right ear and preauricular area mimicking tuberculous lupus. Fusarium oxysporum infection was confirmed by biopsy studies and cultures. The biopsy specimen showed an unusually extensive dermal invasion with fungal hyphae. This is an uncommon clinical presentation for Fusarium infection in a healthy patient. When referred to us, the patient had received antifungal therapy with itraconazole without any benefit. Improvement was obtained with fluconazole therapy. The spectrum of cutaneous involvement related to Fusarium spp. includes toxic reactions, colonization, superficial indolent infection, deep cutaneous or subcutaneous infections and disseminated infection.
Ulcerous lesions disclosing cutaneous infection with Fusarium solani
DOI:10.2340/00015555-0276
URL
PMID:17721650

Fusarium spp. are emergent opportunistic moulds capable of producing life-threatening diseases, usually in immunocompromised hosts. When they infect immunocompetent patients, they usually cause localized diseases. We describe here a case of cutaneous fusariosis in a patient with a medical history of diabetes mellitus and non-Hodgkin's lymphoma who presented with two painful lesions on her left leg. The diagnosis was made on the basis of histopathological findings and skin biopsy culture. The lesions resolved after treatment with oral itraconazole. Cutaneous fusariosis manifests clinically as lesions that can be grouped into a few clinical patterns, and should always be considered in the differential diagnosis of necrotic cutaneous lesions.
Treatment of central venous catheter-related fungemia due to Fusarium oxysporum
DOI:10.1093/clinids/20.3.709
URL
PMID:7756502

We report a case of Fusarium oxysporum fungemia that was related to the presence of a central venous catheter and was confirmed by quantitative cultures and scanning electron microscopy of the catheter hub, subcutaneous segment and cuff, and tip. Despite progressive neutropenia, the infection responded to antifungal therapy within 1 day after the catheter was removed. The removal of the catheter could have contributed to the patient's early favorable response.
A case of Fusarium solani infection under scab of squamous cell carcinoma of skin
Chronic leg ulcer caused by Fusarium solani: a case report and super-microstructure investigation. Chinese Journal of Mycology, 1(4):
Special patient populations: onychomycosis in the diabetic patient
DOI:10.1016/s0190-9622(96)90063-8
URL
PMID:8784304

There are approximately 14 million persons with diabetes in the United States. These patients must cope with the serious complications of this disease, including neuropathy and impaired circulation (leading to the
A case of primary localized cutaneous infection due to Fusarium oxysporum
DOI:10.1007/s11046-010-9290-9
URL
PMID:20177971

Fusarium is a ubiquitous hyalohyphomycete isolated from food, widespread in the environment (plants, soil) and present at all latitudes. Fusarium oxysporum and Fusarium solani are the most frequent pathogenic species, followed by F. moniliforme and F. chlamydosporum. Infections due to this mold may be disseminated or localized. Localized forms include cutaneous and subcutaneous infection, onychomycosis, endophtalmitis, otitis, sinusitis, arthritis, osteomyelitis, and brain abscess. Disseminated forms are those in which two or more noncontiguous sites may be involved. These latter are observed in patients with severe neutropenia. Wounds, digital ulcers, onychomycosis, and paronychia are the typical cutaneous portal of entry. We report a case of primary localized cutaneous infection due to Fusarium in a 29-year-old woman presenting with a nodular lesion, partially ulcerated, asymptomatic on the first finger of the left hand, appeared 4 months earlier. Histological examination showed spongiosis and acanthosis in the stratum corneum, ulceration and inflammation with prevalently mononucleate cells and septate and branched fungal structures in the epidermis and in dermis. The fungus was identified as Fusarium oxysporum by culture of biopsy fragments on Sabouraud dextrose agar with chloramphenicol. The culture was deposited in the culture collection of the mycology section of IHEM, Brussels (IHEM21984 col no. 125). The patient had normal immune status and was successfully treated with surgical excision. Recovery was confirmed at follow-up 8 months later.
Skin infection with Fusarium in an immunocompetent patient
Discrimination of aspergillosis, mucormycosis, fusariosis, and scedosporiosis in formalin-fixed paraffin-embedded tissue specimens by use of multiple real-time quantitative PCR assays
DOI:10.1128/JCM.01185-16
URL
PMID:27605714
[本文引用: 1]

In a retrospective multicenter study, 102 formalin-fixed paraffin-embedded (FFPE) tissue specimens with histopathology results were tested. Two 4- to 5-mum FFPE tissue sections from each specimen were digested with proteinase K, followed by automated nucleic acid extraction. Multiple real-time quantitative PCR (qPCR) assays targeting the internal transcribed spacer 2 (ITS2) region of ribosomal DNA, using fluorescently labeled primers, was performed to identify clinically important genera and species of Aspergillus, Fusarium, Scedosporium, and the Mucormycetes The molecular identification was correlated with results from histological examination. One of the main findings of our study was the high sensitivity of the automated DNA extraction method, which was estimated to be 94%. The qPCR procedure that was evaluated identified a range of fungal genera/species, including Aspergillus fumigatus, Aspergillus flavus, Aspergillus terreus, Aspergillus niger, Fusarium oxysporum, Fusarium solani, Scedosporium apiospermum, Rhizopus oryzae, Rhizopus microsporus, Mucor spp., and Syncephalastrum Fusarium oxysporum and F. solani DNA was amplified from five specimens from patients initially diagnosed by histopathology as having aspergillosis. Aspergillus flavus, S. apiospermum, and Syncephalastrum were detected from histopathological mucormycosis samples. In addition, examination of four samples from patients suspected of having concomitant aspergillosis and mucormycosis infections resulted in the identification of two A. flavus isolates, one Mucor isolate, and only one sample having both R. oryzae and A. flavus Our results indicate that histopathological features of molds may be easily confused in tissue sections. The qPCR assay used in this study is a reliable tool for the rapid and accurate identification of fungal pathogens to the genus and species levels directly from FFPE tissues.
Fusarium infection after solid-organ transplantation
DOI:10.1086/319753
URL
PMID:11283817
[本文引用: 1]

We describe a case of soft tissue infection caused by Fusarium species in a heart-liver transplant recipient, and review the cases of fusarial infection reported among solid-organ transplant (SOT) recipients. Unlike fusarial infection in patients with hematologic malignancies or bone marrow transplants, fusarial infection in SOT recipients tends to be localized, occurs later in the posttransplantation period, and has a better outcome. Surgical resection, when possible, and prolonged treatment with amphotericin provide the most effective form of therapy.
Squamous cell carcinoma arising in longstanding granulomatous hyalohyphomycosis caused by Fusarium solani
Invasive fusariosis: a single pediatric center 15-year experience
DOI:10.1093/jpids/pit080
URL
PMID:26407418

Invasive fungal infection (IFI) is an important cause of mortality in immunocompromised children, particularly after hematopoietic stem cell transplantation. We describe 5 cases of Fusarium IFI in immunocompromised children seen at our institution over a 15-year period. A summary of all published pediatric cases of invasive Fusarium infection is presented. A focus on antifungal management challenges in these patients will be discussed.
The use of ITS DNA sequence analysis and MALDI-TOF mass spectrometry in diagnosing an infection with Fusarium proliferatum
DOI:10.1111/j.1600-0625.2008.00726.x
URL
PMID:18547323

Although mycoses are among the most common diseases worldwide, infections with Fusarium spp. occur only rarely. Mostly patients suffering from underlying immune deficiency are infected with this mould, resulting in a considerably decreasing prognosis. In immunocompromised patients, cutaneous manifestations are more often associated with Fusarium sp. than with Candida sp. or Aspergillus sp. We describe one patient with acute lymphoblastic leukaemia, who was first treated with chemotherapy after GMALL protocol 07/03. After relapse, the patient was successfully transplanted in second remission with a human leukocyte antigen (HLA)-matched unrelated peripheral blood stem cell graft. Ten months later, the patient died from respiratory insufficiency and recurrence of leukaemia. Previously, Aspergillus antigen was detected in blood. In the latter course, disseminated papules appeared. One of these was examined histologically and mycologically. Conventional cultural diagnostics led to the diagnosis of a fusariosis, further supported by internal transcribed spacer (ITS) sequencing and matrix assisted laser desorption/ionisation-time-of-flight mass spectrometry (MALDI-TOF) mass spectrometry, both determining the isolated strain as Fusarium proliferatum, which is a very infrequent pathogen within this genus. Our investigations underline the potential of MALDI-TOF MS based identification of Fusarium species as an innovative, time and cost efficient alternative to ITS sequencing.
Fusarium skin infection: a case report
A 65-year-old man presented with an irregular ulcer with a black eschar on his forehead associated with severe headache. A subcutaneous nodule with a necrotic center was present on the left knee. The diagnosis of Fusarium infection was made and confirmed by biopsy and culture. The patient had a history of bronchial asthma for which he was on inhalational steroids for 5 years. It is unclear if this treatment was related to the disseminated Fusarium infection. The patient received oral itraconazole for 3 months with good improvement but met with an unexpected sudden death.
One case of Fusarium infection of calf was cured by voriconazole combined operation
Objective To explore the clinical and laboratory features of leg ulcer caused by Fusarium moniliforme.Methods Characteristics of Fusarium moniliforme was observed by microscopy and fungal culture.Pathological examination was performed for diagnosis.Results White and cottony mould colony grew on PDA agar at 25℃ with sickle-like macroconidia,concatenate and capitulum-like microconidium under microscope and scanning electron microscope.The fungi was identified as F.moniliforme with the ability growing at 25℃ and 37℃ on Sabrous agar.Chroic granuloma was found,but no fungal components were observed by PAS or silver staining.The lesions were cured after voriconazole and terbinafine treatment combined with debridement and skingrafting.Conclusions A case of leg ulcer caused by Fusarium moniliforme was diagnosed and cured by combination therapy of voriconazole with surgery.
Concomitant amphotericin B therapy, granulocyte transfusions, and GM-CSF administration for disseminated infection with Fusarium in a granulocytopenic patient
DOI:10.1093/clind/16.4.528
URL
PMID:8513060

The use of granulocyte transfusions during amphotericin B treatment of invasive fungal infections in granulocytopenic patients is controversial because of concern about pulmonary complications from leukostasis. Moreover, the administration of granulocyte-macrophage colony-stimulating factor (GM-CSF) to patients with active infections has been questioned because of reports that this cytokine inhibits neutrophil migration into areas of inflammation. We report a case in which the combined use of amphotericin B, granulocyte transfusions, and GM-CSF was safe and life-saving in a pancytopenic patient with disseminated fusarium infection. Histologic evidence of the migration of neutrophils into an area of active infection was found.
Gangrenous necrosis of the diabetic foot caused by Fusarium acutatum
DOI:10.1080/13693780500543246
URL
PMID:16966172

Foot infections are common and serious complications of diabetic patients. We report the case of a 68-year-old patient with a diabetic foot infection that developed into a gangrenous necrosis. Fusarium spp. was isolated on two successive occasions with no other associated microorganisms. Histopathology demonstrated invasion of the fungus into the tisssue. These findings suggested an infection rather than colonization. A detailed morphological study showed that the isolate was Fusarium acutatum, which was confirmed by rDNA sequencing. This fungus is found only in Asia and has not been previously reported as a human pathogen.
Mycetoma caused by Fusarium solani with osteolytic lesions on the hand: case report
DOI:10.1023/A:1015294117574
URL

Eumycetoma is a mycotic disease caused by saprophytic soil fungi that are usually inoculated through minor injuries. A case of mycetoma in a Brazilian farmer aged71 years is reported. This patient presented erythema and edema on the dorsal surface of the left hand with multiple crusted and cicatricial lesions. No macroscopic grains were observed. The histopathological findings showed grains consisted of numerous hyphae which stained well with Gomori-Grocott method. This material obtained by cutaneous biopsy was submitted to culture on Sabouraud’s medium and the colonies were identified as Fusarium solani. The radiological studies revealed bone osteolytic lesions and the ultrasound showed pseudocysts and fistulae at the site of this infection. The patient was treated with oral ketoconazole with a good clinical response.
Cross-reactivity of Fusarium spp. in the Aspergillus galactomannan enzyme-linked immunosorbent assay
DOI:10.1128/JCM.05946-11
URL
[本文引用: 1]

Nine of 11 hematological patients with disseminated/deep-seated Fusarium infection tested at least twice for Aspergillus galactomannan (GM) had repeated positive results in the absence of Aspergillus isolation in culture. The centrifuged supernatants of 12 Fusarium isolates were tested by a GM enzyme-linked immunosorbent assay (EIA). All the isolates produced positive reactions when tested undiluted. These results show cross-reactivity of Fusarium spp. with Aspergillus GM that may constitute a drawback with respect to the specificity of the Platelia EIA.
Use of matrix-assisted laser desorption ionization-time of flight mass spectrometry for identification of molds of the Fusarium genus
DOI:10.1128/JCM.02213-14
URL
PMID:25411180
[本文引用: 1]

The rates of infection with Fusarium molds are increasing, and a diverse number of Fusarium spp. belonging to different species complexes can cause infection. Conventional species identification in the clinical laboratory is time-consuming and prone to errors. We therefore evaluated whether matrix-assisted laser desorption ionization-time of flight mass spectrometry (MALDI-TOF MS) is a useful alternative. The 289 Fusarium strains from the Belgian Coordinated Collections of Microorganisms (BCCM)/Institute of Hygiene and Epidemiology Mycology (IHEM) culture collection with validated sequence-based identities and comprising 40 species were used in this study. An identification strategy was developed, applying a standardized MALDI-TOF MS assay and an in-house reference spectrum database. In vitro antifungal testing was performed to assess important differences in susceptibility between clinically relevant species/species complexes. We observed that no incorrect species complex identifications were made by MALDI-TOF MS, and 82.8% of the identifications were correct to the species level. This success rate was increased to 91% by lowering the cutoff for identification. Although the identification of the correct species complex member was not always guaranteed, antifungal susceptibility testing showed that discriminating between Fusarium species complexes can be important for treatment but is not necessarily required between members of a species complex. With this perspective, some Fusarium species complexes with closely related members can be considered as a whole, increasing the success rate of correct identifications to 97%. The application of our user-friendly MALDI-TOF MS identification approach resulted in a dramatic improvement in both time and accuracy compared to identification with the conventional method. A proof of principle of our MALDI-TOF MS approach in the clinical setting using recently isolated Fusarium strains demonstrated its validity.
Cutaneous infection caused by Fusarium solani and Fusarium oxysporum
Fusarium solani infection of a hypertensive leg ulcer in a diabetic
DOI:10.1111/j.1439-0507.1980.tb02568.x URL PMID:7464854
Exome sequencing reveals a signal transducer and activator of transcription 1 (STAT1) mutation in a child with recalcitrant cutaneous fusariosis
DOI:10.1016/j.jaci.2012.11.005 URL PMID:23245795
Cutaneous Fusarium moniliforme infection. Master’s Thesis,
A case of chronic cutaneous ulcer with infection of Fusarium moniliforme under crust
Pyoderma gangrenis: a case report
Onychomycosis caused by Fusarium solani in a woman with diabetes
DOI:10.1111/j.1365-2230.2009.03498.x
URL
PMID:20055843

A case of untreated fusarial onychomycosis leading to serious consequences is reported. Fusarium solani is a widespread fungus and an occasional human pathogen. It usually invades rapidly in immunocompromised hosts, and often results in a poor outcome despite treatment. We report a woman with diabetes mellitus who had untreated fusarial infection of the nails, which developed into subcutaneous fusariosis, superinfected by bacteria, and then evolved into osteomyelitis that subsequently resulted in septic shock. Early management of mycotic nails in immunocompromised hosts is crucial to prevent life-threatening disease.
A case of lower extremity ulcer caused by Fusarium solani
Fusarium solani infection of cornea, perioral area and genitalia in 3 cases
Mycetoma of the foot caused by Fusarium solani: identification of the etiologic agent by DNA sequencing
DOI:10.1128/jcm.41.4.1805-1808.2003
URL
PMID:12682194

We report a case of Fusarium solani mycetoma of the foot that could not be diagnosed by culture, but was correctly identified after amplification and sequence analysis of fungal internal transcribed spacers 1 and 2 and 5.8S ribosomal DNA regions.
Fusarium graminearum causes cutaneous fusarium disease
A case report of skin Fusarium sp. granuloma
小儿面部镰刀菌感染1例
由胶孢镰刀菌所致足部皮肤无色丝孢霉病一例
茄病镰刀菌致足部透明丝孢霉病1例
目的 报道1例茄病镰刀菌引起的足部透明丝孢霉病。方法 询问病史及体检,取足部的皮损行皮肤病理检查、真菌培养及致病菌的形态学观察、鉴定。结果 致病菌为茄病镰刀菌,给予局部病灶切除及伊曲康唑治疗,随访3个月,病灶明显缩小。结论 本病例证实为茄病镰刀菌引起的足部透明丝孢霉病,经口服伊曲康唑及局部病灶切除治疗,疗效明显。
茄病镰刀菌致皮肤透明丝孢霉病1例
异基因造血干细胞移植后茄病镰刀菌感染一例并文献复习
目的 提高对免疫低下患者茄病镰刀菌感染的认识,探讨治疗方案.方法 报道1例急性髓性白血病异基因造血干细胞移植后合并茄病镰刀菌感染患者的临床表现、治疗经过和转归并进行文献复习.结果 患者男,46岁,于干细胞移植术后出现肺部浸润影及全身多发性皮下包块,组织涂片见大量菌丝及孢子,真菌培养为茄病镰刀菌,行皮下包块切开引流,两性霉素B及伏立康唑抗真菌治疗,恢复后痊愈出院.以"造血干细胞移植"或"异基因造血干细胞移植"或"骨髓移植"+"茄病镰刀菌"为关键词在Medline和中国生物医学文献光盘数据库中进行检索,未发现中文报道,国外文献报道7篇,共8例,其中男5例,女3例,主要临床表现为发热及全身皮肤损害,预后极差,8例中7例死亡,1例治愈.结论 茄病镰刀菌感染是造血干细胞移植后少见的、致死性的并发症,应引起足够重视,对异常皮肤损害或皮下包块应尽快行组织涂片及培养,早期明确诊断并给予足量抗真菌治疗.
儿童急性淋巴细胞白血病并发镰刀菌败血症
串珠镰刀菌引起小腿溃疡l例
红斑肢痛症继发尖孢镰刀菌感染1例
足部皮肤镰刀菌病
茄病镰刀霉引起皮肤透明丝孢霉病1例
儿童皮肤串珠镰刀菌病
皮肤鳞状细胞癌痂下滋生茄病镰刀菌 1 例
茄病镰刀菌致小腿慢性溃疡1例报告及病原真菌超微结构的研究
伏立康唑联合手术治愈小腿镰刀菌感染1例
目的 探讨串珠镰刀菌致小腿溃疡患者临床及实验室特征。方法 多次取患者溃疡分泌物作直接镜检和真菌培养,观察真菌形态学特征。取皮损组织病理活检。结果 在马铃薯培养基中25℃培养均长出白色棉絮状菌落,显微镜及扫描电镜下见大分生孢子呈镰刀状,小分生孢子链生和假头状着生并存,在沙堡琼脂25℃和37℃均生长良好,经鉴定为串珠镰刀菌。组织病理学显示为慢性炎性肉芽肿改变,PAS及六胺银染色均未见真菌成分。伏立康唑联合特比萘芬治疗有效,整形外科清创植皮后治愈。结论 确诊1例串珠镰刀菌引起的小腿溃疡,伏立康唑联合手术治疗皮肤镰刀菌感染疗效好。
皮肤串珠镰刀菌病
慢性皮肤溃疡痂皮下滋生串珠镰刀菌1例
坏疽性脓皮病1例
茄病镰刀菌引起下肢溃疡1例研究
茄病镰刀菌感染角膜、口周、生殖器3例
禾谷镰刀菌致皮肤镰刀菌病
镰刀菌皮肤肉芽肿1例